This article was featured in One Great Story, New York’s reading recommendation newsletter. Sign up here to get it nightly.
Let’s begin with an action scene: I was in midair, tumbling sideways, heading for the floor of the Columbus Circle subway station. Not a place I wanted to be. Where I wanted to be was on the downtown 1, five or ten yards away, doors standing open. I’d made this connection more than a thousand times, though usually getting off the 1, not on it.
This time, I was out of practice and I got it wrong. After stepping off the downtown B or C, I took the wrong stairway and had to double back to get over to the right side of the 1. When I climbed up the correct stairs, the stairs I used to fly down every morning, straight from the optimal train door on my precisely plotted commute, I saw the 1 arriving.
And then — well, if I knew exactly what happened, it wouldn’t have happened, would it? What I registered went like this: I sped up, or I meant to speed up. Someone cut across my path. I tried to steer around them and my legs … my legs did something else. Or did nothing. The extra walking and climbing had taken too much effort, and my intentions lost contact with my legs. I reached out and tried to brace myself on someone’s shoulder; they were wearing a black-on-white shirt; I was so undone I was trying to make physical contact with a total stranger on the subway platform. I missed. All that was left was to hit the station floor, so I did.
I rolled to my knees and discovered that was as far as I could make it. My legs couldn’t get me upright again. One guy streaming by broke stride, asked if I was okay, and hauled me to my feet. I checked myself: no torn clothes, no blood. Another 1 was pulling in, one minute behind the train I’d missed. I got on and went where I’d been going. I had just had a fall.
Old people have falls. I had only just turned 52 one week before the September evening I collapsed. But the year from 51 to 52 had been a remarkably bad one. I gambled on a job I wanted, as the editor-in-chief of a small magazine, and it ran out of funding. I sent applications to other publications and got thoughtful rejections. I sent more applications, and they went unanswered. I made an appeal for paid subscriptions at a newsletter I’d been writing. Its revenue flattened out at about 20 percent of my share of our living expenses. The household finances began to drain.
I picked up an adjunct gig, teaching a writing class on Zoom, three straight hours a shot, and the anxiety of filling the time — of giving the students what they were paying for — gathered into a lump in my upper torso until I couldn’t stand the taste of the herbal tea that was supposed to relax me and give me something to do with my hands on-camera. My shoulder locked up. I got pins and needles in my arm.
What was happening to me? I don’t go looking for medical-mystery articles in the newspaper, but when I see one, I read it end to end. The strangest things happen to other people’s bodies! Someone, if I remember right, fought a lingering cough for years because they accidentally inhaled a pea and forgot about it. The medical-mystery column has a beginning and a conclusion. In between is a fumble for clues, moving toward a flash of insight. Some doctor finally runs the right test, recollects the right journal article. The shapeless misery takes shape.
I went to see a shoulder specialist. He knew exactly what was wrong. I had trigger points, little knots in the muscle under the shoulder blade. He gave me some exercises — pin a tennis ball between the shoulder and the wall, lean back, and roll around on it — and a prescription for an anti-inflammatory. A few days later, I noticed my shoes were laced too tight when I tried to put them on. Another day and I made the connection: No, my feet were too big for my shoes. Google said that anti-inflammatories can cause swelling in the extremities, so I stopped taking the pills.
My feet kept swelling, day by day, until my pink ankles looked like deli hams and I started using a butter knife as a shoehorn. I’d reluctantly spent some money to order a new pair of canvas sneakers, off-white, for the spring and summer, and I left them in the box, unable to face the thought of jamming my distended feet into them. The pins and needles spread to both arms, like I’d slept on them funny, except the sensation lasted all day.
I could still type through the numbness, though, publishing what I could for what money I could get. I stopped buying myself things that seemed discretionary — the good oolong tea leaves, crushproof imported pocket notebooks, a new pair of jeans — but some spending had its own momentum. My wife’s family had booked an Airbnb in Italy for April. It would be our first vacation since before the pandemic, our middle-schooler’s first trip abroad since he was in an infant seat. It would have been absurd to cancel just because I was between jobs. My ankle ached on the clutch pedal of the rented Fiat. I brought along a folder of unfinished tax paperwork. The amount I owed the IRS would match, almost exactly, a big freelance check I was waiting on. The deposit went into and out of my account on the same day.
I went to my regular doctor, whom I’d bypassed on the shoulder thing. He was baffled at the symptoms and frank about his bafflement. Swollen feet can mean congestive heart failure, so he referred me to a cardiologist. She instructed me to walk and then run on an inclined treadmill, hopping on and off for ultrasound imaging of my heart. I have — had — always been extremely healthy without being physically fit, so while I didn’t enjoy the test, I still passed handily. My heart was strong and well.
Sometimes this kind of swelling just happens and then goes away, the cardiologist said. Whatever it is, you won’t die of it.
I’ve told the story over and over, to various doctors, till it almost sounds like a coherent narrative. When I drafted this passage, in the dark, by thumb, on a phone plugged into the USB socket of a hospital bed, I’d been telling it to several people a day: general practitioners, neurologists, rheumatologists, radiologists, nurses, physical therapists, medical aides, a dietitian, a surgeon. The story, I told them, happened in two parts. In the spring and summer, part one, I chased the swelling and numbness and other symptoms — stiff fingers, shortness of breath, tightness in the chest — in slow motion from doctor to doctor. Mostly, this was shepherded by the cardiologist, who seemed to feel as if, by ruling the problem not to be her business, she had made it her duty to discover whose business it might in fact be.
I saw a neurologist, who talked me into spending $700 from our high-deductible health plan on getting my muscles zapped with a little Taser and told me the results said I had carpal tunnel. I did have carpal tunnel, but not really, not because my terrible ergonomic habits had caught up with me. The swelling had simply gotten into my carpal tunnels for a while. I ignored his suggestions for exercises and supplements, and months later, in the hospital, I got an email telling me his practice was going out of business.
I saw a rheumatologist. He ordered a bunch of blood tests and suggested I take prednisone and something else. When I opened the paper bag from the pharmacy, I realized the something else was hydroxychloroquine, the malaria drug that had a moment in the news as a spurious COVID treatment. I took only the prednisone. My ankles stayed puffy. You could jab a finger into one and leave a dent that lingered.
Before this, my hands had been loose-skinned and a bit wrinkly, the one part of me going more visibly on ahead through middle age than the rest. My hands looked like my mom’s hands, and I would catch myself gazing at them sometimes and congratulate myself on my resignation to the realities of aging, the mortality of all flesh. Now my fingers resembled Italian sausage links, tight and shiny, with no reassuring philosophical overtones at all.
One symptom would fade and a new one would assert itself. My ankles deflated and I started wearing the new sneakers, but my breathing and stamina steadily worsened. A wheeze or cough would interrupt my talking. On the mile-long walk back from school with my younger son, the route we’d been taking for two years, I lagged behind, guiltily asking him to slow down. I started buying five-pound bags of rice from H Mart instead of ten-pound ones. Then I just started getting rice delivered.
Nobody cracked the puzzle. The folder of referrals and results I carried to appointments got thicker. My blood tested positive for signs of general inflammation and negative for the constellations of markers that would point to any particular inflammatory condition. I had not been bitten by any ticks; I had never gotten the Lyme rash or any other diagnostically meaningful rash. My fingers did not exhibit a telltale sign of turning stark white when they got cold. My chest X-ray and CT scan were clean. The closest thing to a breakthrough was basically an accident: During a routine vitals check, a nurse asked if I was holding my breath. I was sitting still, and my pulse-oximeter reading was refusing to go over 95 percent.
Normal is 95 and above. Below 90 is an emergency. I self-tested at home with a device on my finger. Light activity, like bustling around the kitchen, would knock my level down to 91. Walking a bag of groceries home and up the stairs dropped me to 87. At a medical center, I did breathing exercises with a mouthpiece in a sealed booth. I passed that test. I went to a pulmonologist and passed every test there, too. If you ignored the pulse-ox readings, my lungs and heart were, officially, fine.
There was zero explanation; there was, maybe, the absolutely obvious explanation: that I was stressing myself into this over money. We’d been absorbing plenty of strain in the household before I lost my job — some normal midlife stuff, some normal parent stuff, some abnormal and menacing stuff that I truly can’t even get into. Our black cat gnawed our potted prosperity bamboo to shreds. Trying to save it, we overwatered it until it rotted from the inside out.
It had not been the wisest time to choose an unstable job in a beyond-unstable field. If my time as an editor-in-chief had even been a job: I applied for unemployment, got rejected, and after months of appeal, the State of New York ruled that my past two full-time situations had been contract gigs, uncovered. I considered whether my illness could be a conversion disorder flowing from my misguided career choices. On some level, I believed the swelling would go down and the oxygen would go up as soon as I collected a few consecutive pay stubs from a normal, salaried job.
Back in the winter, I’d met up with a friendly fellow writer who happened to have just secured, through a different line of work, an amount of money that meant financial security forever. In theory, we were talking about ways to fund the job of mine that was about to run out of money, but we both knew that wouldn’t happen. “You’ve got a good reputation,” he said. “Someone will want you to work for them.”
This had been true enough before. I’d made myself a useful editor and a reasonably well-known writer over the years. I moved between jobs without much trouble, tending to get hired the way murderers in movies get hired: a message or phone call from someone who needed something done and who thought I could do it. Abruptly, all that my connections could offer were gigs. Someone needed a manuscript edited before they gave it to their book editor. A magazine wanted a book review. Work, but no jobs.
I kept applying for something stable. A notoriously lavish start-up loved my proposal for a mini-section within its soon-to-be-launched vertical until the sponsorship for the vertical failed to come through. A major media company advertised for a position that exactly fit my history, then withdrew the listing in the middle of an executive meltdown. A friend of a friend let me know that another major media company was ignoring my application because it wanted someone less opinionated. I started calling in favors, nagging people with whom my friendships had previously been non-transactional. It broke up the dead silence, at least.
My wife and I considered disaster scenarios in which the “disaster” was simply that things kept going the way they were going. We did the math on vacating our condo, finding tenants, and living in a cheaper rental. Maybe it was time to leave New York. But it wasn’t clear if we had enough savings to cover such a move. It wasn’t even clear if I had the physical energy to pack boxes. On the online job forms, there was usually a question about whether I, the applicant, identified as disabled. I paused longer and longer each time. Disabled? I was … less able. To do things. Than I’d been. For now? I clicked “no,” uncertainly.
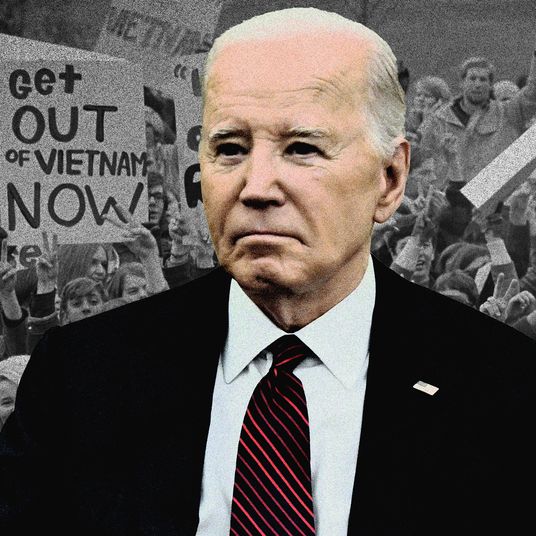
Part two of the story is I got COVID. I’d avoided it for three years, but everyone is going to contract the virus sooner or later. It’s not worth the trouble, officially, to even politely suggest people should wear masks or to keep the public up to date on the rate of new cases. The pandemic is over, people keep on saying. You are free to make your own decisions about what risks to take individually without any useful information about the overall risk picture.
I’d been furious about this already on other people’s behalf. Most Americans, the Biden administration said, would be fine if they were vaccinated. This elided the people who wouldn’t be: the immunocompromised, for example, and those with certain respiratory conditions. The political and journalistic consensus had set the value of these people’s safety at zero, not even granting them the benefit of mask advisories or ventilation standards.
When I started hearing about the late-summer COVID wave, it occurred to me that now I was one of those people myself. This is what disability advocates have said all along, not that it usually sinks in: The able and the disabled aren’t two different kinds of people but the same people at different times. Last year, I was healthy; this year, I had a breathing ailment, even if nobody could say exactly what that ailment was.
I got Paxlovid delivered and sank into fever. The back of my throat was so raw I would wake up snorting for air. Rolling around in my bed, I felt, for the first time, that this body of mine truly was going to die someday. Not the abstract knowledge that death awaits all of us but the shocking awareness that eventually this system of veins and nerves and organs would lose its familiar stubborn equilibrium, cease functioning, and fail. I fixated on whales. They’re right out in New York Harbor. What if I used up my allotted time on the planet without ever laying eyes on a whale? I booked a whale-watching cruise for the family. Later, when the day came, it got canceled by a hurricane.
In August, when the acute COVID infection ran its course, I got out of bed and back on my feet. But after a week or two on the upswing, a whole new set of malfunctions took over. Routine movements burned as if I were doing deep stretching. I couldn’t get through a meal without a coughing fit from a lump of food getting stuck or a drink of water splashing the wrong way. Saliva accumulated in my mouth till I had to go to the sink and spit. I ate more slowly and stopped getting seconds, feeling like I was in one of those testimonials about the new anti-obesity drugs, in which people tell how their motivation to keep eating has disappeared. I was far past needing or wanting any weight loss. My sedentary midlife flab had long since ebbed away, and now I was losing something else, down ten pounds in a month. Maybe, the cardiologist said, eyeing my scrawny limbs and loose clothes, I should consider checking into a hospital. Just so I could get all my testing coordinated in one place.
It was only a thought, one that dissipated as I sought out second opinions. The medical-mystery column doesn’t usually dwell on how slowly the inquiry goes in our fractured health-care system. How the highly recommended pulmonologist doesn’t return the first phone call and only has an opening five months away, and how the major-medical center does have an appointment but isn’t in network with the major-medical insurer. How the chest X-ray is over by the East River and the breathing booth is in the West 160s and the phlebotomist is by Columbia, and how each one has its own online portal for billing and results.
Every day, my legs were harder to move. Climbing in the door of an SUV, I couldn’t lift my rear foot over the threshold until I reached down with my hands and pulled it in. Then the grab-and-lift maneuver became necessary to step into my pants. I had to ask the kids to pull pots and cutting boards out of the bottom kitchen cabinets for me. I gave up bedtime-story duty, crawling into bed each night before anyone else, half-hearing my wife’s voice reading in the next room, feeling myself fading out of my own life. I imagined living in a world and a class where a person could retreat to a sanatorium and shut everything down until the problem was figured out.
I stopped leaving the apartment. The project of washing left me needing to lie down. One morning, or possibly afternoon, it took me four or five tries to shrug my way into my bathrobe, nearly overcome by the weight and friction. I gave up on shaving, and the rattiest stubble of my life took over my chin. The kids were put in charge of the cat box because I couldn’t reach that corner of the bathroom anymore, but one night I got down on the floor to help and when we were done I couldn’t stand up. I didn’t even know how to start to try. Eventually, my wife grabbed me under the armpits from behind and hauled me most of the way upright while I gabbled warnings about my legs giving way.
Two different realities or images stood superimposed in my mind. There was the body I’d occupied two months ago — my body, as I understood it — walking over to Broadway for pizza, taking the younger boy to the basketball courts, ducking into Central Park to climb the Great Hill. And then there was Andrew Wyeth’s Christina’s World, a gaunt figure dragging her useless legs along the ground. If this was histrionic or self-pitying, it seemed less so on the days when I couldn’t raise my hips up off the floor. The only thing that still felt more or less normal was sitting at a desk, doing the work I was trying to get someone to pay me to do.
Meanwhile, in the span of time that it took a newspaper to move one step down its hiring checklist from a Zoom interview to an edit test, a law school in a small southern town progressed from sending my wife a preliminary inquiry to making her a tenured job offer with a part-time teaching slot for me thrown in. We booked a visit for the family to see if we could really live there. As the trip came closer, we realized there was simply no way I could walk through an airport. The rest of the family would have to scout out our possible future while I stayed home.
As they prepared to go, my GP called with the results of my latest bloodwork. A normal range for creatine kinase, a marker of muscle breakdown, might be between 30 and 200 units per liter. A new test said my level was 8,000. The reason my muscles felt so weak was that they were actively dissolving into my bloodstream.
I wrapped up a job-recruiting call, threw my glasses and contact-lens case into a shoulder bag, and booked an Uber to the emergency room. My wife took my sons to see about the job. It was unclear which of us was going to the place that would offer a solution.
In the hospital, the medical mystery falls into an awkward, indeterminate zone. Between the fall and the choking and the creatine kinase, my story qualified me as a definite emergency when I shuffled up to the admission desk. But it was a conundrum to be solved, not as straightforward and urgent as a stroke or broken hip. The staff put me in a wheelchair and parked me in a walkway lined with other people in wheelchairs. The hospital was beyond full. There were genuinely not any open beds, not only as an administrative category but as literal objects to lie down on. I spent my first night on a gurney in the ER observation section, fully dressed and still in my shoes. To avoid catching anything else, I kept a mask on, the elastic digging into my ears.
On the second day, I got a bed and changed into two layers of hospital gowns. My clothes and my new sneakers went into a pair of plastic patient-possession bags. Doctors came by, individually and in teams, with blue gloves on, to test my muscles. Squeeze my fingers. Push up against my hand with your knee. Stick out your elbows and don’t let me push them down. The closer the blue gloves came to the middle of my body, the worse I did.
The doctors had questions. Had I been hiking at all back in the spring, when my troubles started? No? Was I sure? Not even in Central Park? This was about Lyme disease again, of course. I knew about Lyme, and the ever-growing literature of people’s struggles with Lyme, and the whole elusive post-Lyme complex. But I also still knew, as solidly as I could know any fact about my health, that I had not been bitten by any ticks. One doctor after another asked me to blink my eyes, harder, over and over, watching for the lids to droop from fatigue, which might mean myasthenia gravis. My lids did not droop.
ER time took over, with “day” and “night” merely more or less busy spells in an unbroken atmosphere of fluorescent lights and beeping. A 24-hour flight in coach, a 48-hour flight in coach, a 72-hour flight in coach. The patient behind the curtain to my right kept his TV blaring all night, cycling episodes of the same forensic true-crime show: some ghastly rape or murder, the bafflement of investigators, the infallibility of scientific evidence coming to the rescue. The Kars-4-Kids jingle playing in between.
My obvious risks — choking, falling — had standard countermeasures: puréed meals and caution-yellow nonslip socks with a matching wristband that read FALL RISK. For treatment, there was nothing but big bags of IV fluids to flush out the creatine kinase while keeping my underlying symptoms untouched, the better for accurate testing and observation. The creatine kinase went down to 5,000, back up to 6,000, down again. The staff rolled me away to a chest X-ray, a thyroid ultrasound, a contrast CT scan, an MRI. Wheeling down the hall toward an echocardiogram, I passed the neurology team going the other way, misconnecting on a planned meeting. I never talked to them again.
A real hospital room, outside the ER, opened up in the late afternoon on the fourth day, a Saturday. It was on the tenth floor with a window looking uptown over the top of Central Park. I could see the boathouse by the Harlem Meer, but not the water itself, because the trees were so thick and green. I wondered, tempting fate, what it might look like when the colors turned.
My new roommate, a friendly, stooped figure, was in agony for non-mysterious reasons — a manageable condition that had gone unmanaged because the treatments cost too much money. The problem-solving sessions on his side of our shared curtain, with the doctors and social workers, were about which programs or policies might help him if he and his family could sort them out.
For me, evidence and theories kept trickling in. Doctors would come by and mention some finding, or my phone would give an automated notice that a new lab result had arrived and I would Google as best I could. Open tabs accumulated on my phone: RNP antibodies, rheumatoid arthritis, polymyositis, mixed connective tissue disease. (“The overall ten-year survival rate is about 80 percent.”) I was negative for hepatitises B and C, negative for Sjögren’s-syndrome antibodies, negative for syphilis, negative for Lyme (told you) — negative for most things, as I’d been all along. The speed with which my muscles were falling apart seemed to be, in some sense, good news, meaning that I probably wasn’t going through one of the more gradual neurological degenerations like ALS.
Down in radiology, I took a swallowing test, a three-course flight of barium snacks: a thick barium drink, spoonfuls of barium marshmallow fluff, then bites of the barium fluff on a graham cracker, consumed one after another on live X-ray video. There was my jaw, my tongue, my hyoid bone, and there were clots of barium-tinged food getting visibly hung up short of the esophagus, behind the tongue, in little pockets of underperforming pharyngeal muscle. None of the food, however, was obstructing my windpipe. It meant I was eligible to trade in puréed green beans for individual green beans, French-toast paste for ordinary French toast.
A provisional unifying idea took shape. More and more, the conversations circled back to one form or another of myositis: an autoimmune attack on my proximal muscles. If the muscles were the essence of the problem, then my oxygen troubles could have been a muscle problem all along too, a creeping weakness in the diaphragm. The swallowing trouble would be the muscle problem appearing in the pharynx. The swollen ankles and knuckles — well, those weren’t quite muscle problems, but they also were no longer a pressing concern. What I needed, urgently, was a muscle biopsy, one that might tell the doctors exactly how that part of me was going wrong.
It was my bad luck, the attending doctor said at my bedside, to be an interesting case. Our meetings had a tone of rueful amusement. Yes, I was in pain and reeking from infrequent showering, but we could talk about the unresolved mystery and its submysteries with a certain detachment. My oxygen levels were behaving themselves. No one knew where that problem had gone, nor why my voice had suddenly gone faint and reedy.
My wife was back from the job-scouting trip, but she’d picked up a foot infection and was stuck in the apartment, taking antibiotics. The boys trooped across the park to bring me my laptop. They were visibly alarmed by how gaunt and shaky I was. I took them on a shuffling tour to a long back hallway lined with sleek, derelict equipment, with a window facing out on a black monolith of a building, to show them how much it looked like Andor. We shared the crunchy, startlingly good French fries on my dinner tray. I couldn’t have swallowed that many on my own.
Now that I had the computer, I rummaged through test results and image scans on the hospital information portal. I could navigate this way and that through the inside of my own body on the CT or MRI files, moving the cutaway to watch the stark white rib cage flow into the spine. My thoracic aorta was “normal in caliber and course.” My right iliac bone had a “tiny sclerotic focus” that was probably a “bone island.” My muscles were all fucked up:
Diffuse STIR hyperintense signal throughout the visualized musculature of the pelvis and thighs as well as partially visualized portions of the paraspinal muscles of the lower back, including the quadriceps muscle (vastus lateralis, medialis, intermedius), hamstrings, iliacus, psoas major, gluteus medius and minimus, pubococcygeal muscles, adductor muscles, highly suggestive of systemic myositis in the appropriate clinical setting.
I knew this, implicitly. It was apparent every time a nurse or technician asked me to scoot a little in my bed and my psoas major or adductor or the rest simply wouldn’t do the scooting. The most minimal movements were the most impossible. It was easier to clamber out of bed, take a six-inch step, and clamber back in at the new spot than to shift my body. If my pillow slipped down to the small of my back, there was no retrieving it.
A perverse rule of medical technology is the more you scan, the more you discover, whether those discoveries matter or not. The imaging reports noted a “small hiatal hernia”: Google said a weakened diaphragm could cause that. I had an “underdistended stomach,” as would anyone who was expected to eat French-toast paste. My liver was “prominent in size,” which qualified as “hepatomegaly.” My lower lungs had “minimal mild reticular opacities.”
One discovery was notable, or might have been. A night-shift doctor brought it up offhandedly, as if someone else must have already mentioned it: The ultrasound had picked up a nodule on my thyroid. Could it be squeezing my trachea? Could it be cancer? Could it be nothing? Sure. A little more inspection and the nodule became nodules, plural, the largest being a nearly inch-long sausage on the thyroid isthmus, salient and crying out for analysis. The thyroid-biopsy team swooped in during lunchtime, chatty and armed with portable gear for working at my bedside. One person tracked down the sausage with an ultrasound wand against my neck while another jackhammered away at it with a tiny needle. They prepared the samples in little vessels of brightly colored liquids laid out in the sun on the windowsill. The technicians eyeballed the cells on a microscope set up in the hallway and declared that nothing looked obviously malignant. My thyroid itself, they said, showed “lymphocytic thyroiditis.” Also known as Hashimoto’s disease, although who could say, here, whether it was a disease unto itself or a manifestation of some greater disease. The question was bigger than the thyroid.
Now there was almost nothing left to do but the muscle biopsy. Ten stories up turned out to be cruising altitude for hawks, wheeling by the window in the sunlight, borne along on the fresh autumn breezes. I gave my daily samples of blood. I sent some follow-up emails about jobs. The procedure was scheduled for Thursday, my ninth day in the hospital, in the last slot of the afternoon.
As the time came closer, I began to apprehend an uncomfortable truth. The actual medical mystery wasn’t about anything inside me. It was whether the tests were going to point to some far side of this where I got my life back. Was there a future where I could walk out the door on Sunday morning in decent shoes and make it to church? Where I could pick up heavy groceries to put a three-course meal on the family dinner table? Where we could rent a rowboat? Where I was a helpful and economically viable member of the household?
The operating team drew a mark on my right thigh and put me under sedation. When I came around, I was still in the operating room. My wound was neatly sewn up but the team was on the phone with the pathologists, who wanted to discuss whether they’d taken a big enough chunk of my leg. Pleasantly high and feeling fantastic, I assured everyone it was fine if they wanted to go back and get more. You know — While we’re here, happy to oblige. They decided against it, and off I went to recovery. It was the nicest feeling I’d had in weeks. I looked at my hands and I could believe the old familiar wrinkles were coming back.
Later on, it felt as if someone had sliced open my thigh, since they had — an additional stabbing pain tucked inside the usual burning pain when I used my quadriceps. But that was tolerable. I was finished with being a test subject. All the possible diagnoses pointed to the same treatment, anyway, so the next morning, I got a syringe of steroids pushed into my IV, chased with a cold squirt of saline to make sure every drop went through. I was a patient, trying to get well. Within hours, maybe, my thigh muscles seemed a little less dead than before. That afternoon, I limped off to the bathroom, pulled the shower chair out of the shower, and sat down to make a job interview call, away from any beeping machines or doctor visits. At least it wasn’t a Zoom.
Out the window, I could see magenta and gold in the tree canopy of Central Park. It was deep enough into October for that now. My creatine kinase dropped from 6,200 to 4,500 overnight, then headed for the 3,000s, a level a person could go home with. Whatever had made my immune system start tearing up my muscles, the steroids seemed to be making it slow down. That’s what they were: immunosuppressive drugs, to be followed over time by other, different immunosuppressives. If all went well, I would trade being an actively sick person for being an immunocompromised one.
The blue-gloved muscle checks resumed. Oh, yes: Much stronger in the legs. I took a lap around the ward. I spent less time in bed and more in a chair. I booked another job call with maybe some steroids-laced overconfidence. My wife, with a counteroffer from her current employer in hand, turned down the southern school.
Normal life, or whatever would stand in for normal, was calling. On my 15th day, with the pathology report on my leg sample still a work in progress, the last sparkling dregs of a fat bottle of immunoglobulin filtered into my veins. The two-day infusion was the final piece of treatment that had required hospital care. I was free to go. When the IV came out of my arm, I dug out my things from the closet and got dressed. Clean pants and a clean T-shirt over my poorly cleaned body. My eyes in the mirror were sunken, my neck withered. Nonstop mask wearing had scraped the bridge of my nose raw, and my ratty stubble was now a full ratty Vandyke, the chin shot through with gray. I peeled off my last pair of grimy yellow nonslip socks and wrestled my way into my own regular socks.
Now the shoes. I’d been imagining how this would feel for days. I reached into the hospital bag for my canvas sneakers and pulled them out. They were mashed out of shape and … damp to the touch? Damp to the touch. Had something spilled into the bag, somehow, or was it just residual sweat? Either way, they had been sealed in plastic with it for two weeks. Flecks of mold had sprung up on the otherwise new-looking insoles.
There was nothing to do but wear them. I would be taking myself home. The hospital had sent my prescriptions to the nearest pharmacy for me to pick up on my way out. A string of robocalls and human calls then informed me that the branch did not, in fact, have all the meds I needed, specifically the steroids. My wife headed across town to another location, where the computer indicated there were enough steroid pills to last me three days.
The nurse who’d unplugged me reappeared with a sheaf of papers: I was discharged. No final consultation with any of the doctors. The nurse asked if I wanted a wheelchair. I figured I might as well start walking.
By the time I reached the ground floor of the hospital with my bags, I understood that had been a mistake. My room had been on the west side of the building; the pharmacy was on the east, an entire avenue over. I walked a few yards down the vast hallway, paused for a stricken moment, then walked a few more. I couldn’t wipe out again. Stopping and going, I made it to the east side of the building, down a short flight of steps, and out. Numbly, I trudged up the sidewalk in the quickly fading twilight, clutching my papers. It dawned on me that I still didn’t have a diagnosis.
I despise those stories where a writer tells you all about some mystery for thousands of words and then fails to deliver the solution. Usually with some metaphysical vamping about the unknowability of all things. What are you even telling anyone about it for? But I didn’t have an answer, and I still don’t. It would be more than another week before the pathology report came back. My muscles, it said, showed “myopathy with scattered necrotic myofibers in the absence of significant lymphocytic inflammatory infiltrates.” I couldn’t raise a doctor on the phone to talk about it. Whoever wrote the report had floated a whole new possibility, “antisynthetase syndrome,” to go with the other possibilities still bobbing around. The hospital rheumatologists, weeks later, would stick with polymyositis; a different myositis expert would propose “immune-mediated necrotizing myopathy.” A neurologist would suggest “lupus-myositis overlap syndrome.”
Medicine hasn’t really solved for the body attacking itself. Since the inflammation first brought me to the rheumatologist months before, I’d been quietly bracing for an answer that wouldn’t feel like an answer. An authoritative-sounding name like scleroderma would come up, and Googling would fill in non-detail details like “no cure” and “symptoms vary” and “don’t know exactly what causes this process to begin.” The thing that had taken me apart was something rare and diffuse, its effects almost certainly melded with those of the coronavirus. I was on my own with it. I was three weeks behind on a freelance editing gig, and November’s bills were cycling into view. In January, an endocrinologist had an opening to see about my thyroid.
The pharmacy window was, as pharmacy windows are, all the way at the back of the store. An incredible distance. A terrifying distance, alone on my shaky legs. I put out a hand to steady myself against the shelves along the way, and waiting in line I just grabbed on. I said my name to the pharmacist as clearly as my cracked voice could muster, got the pills, and retraced the long path to the door.
It was fully night now. As I stepped outside the pharmacy vestibule, I saw an empty taxi coming up the block, preparing to turn the corner. Memory and instinct said it was mine: Two or three long, quick strides to the curb and a sharply upthrust hand would catch the driver’s eye. My body knew otherwise. I ventured a short step, not even to the middle of the sidewalk, and the taxi went on by my half-raised arm.