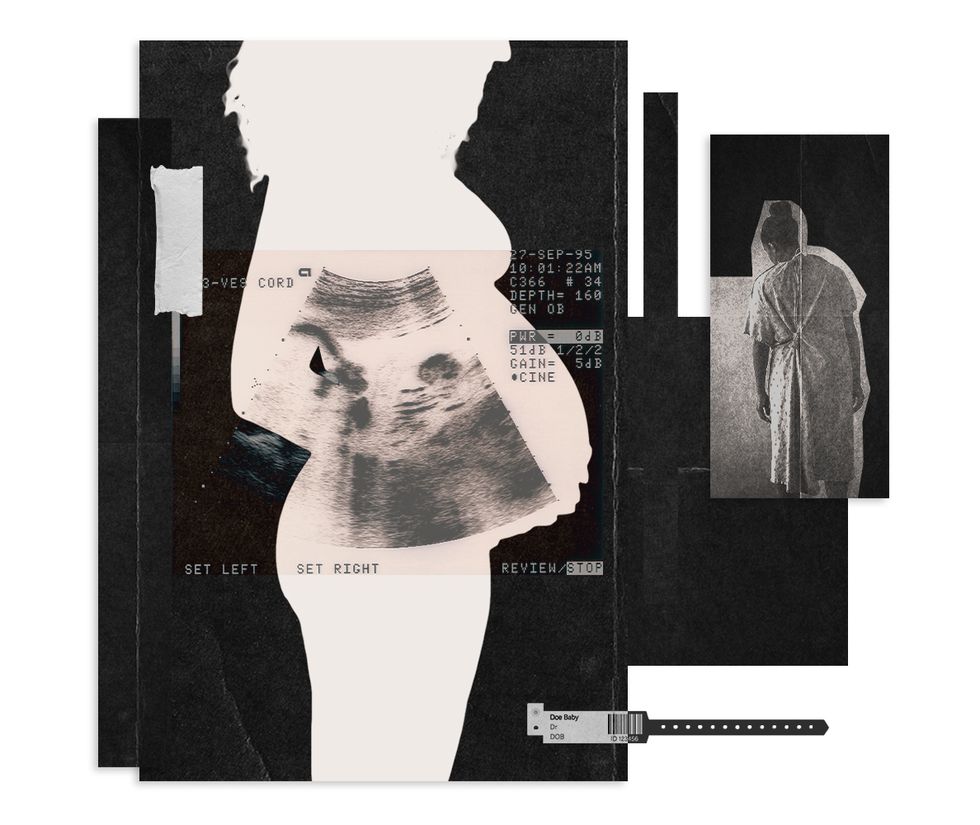
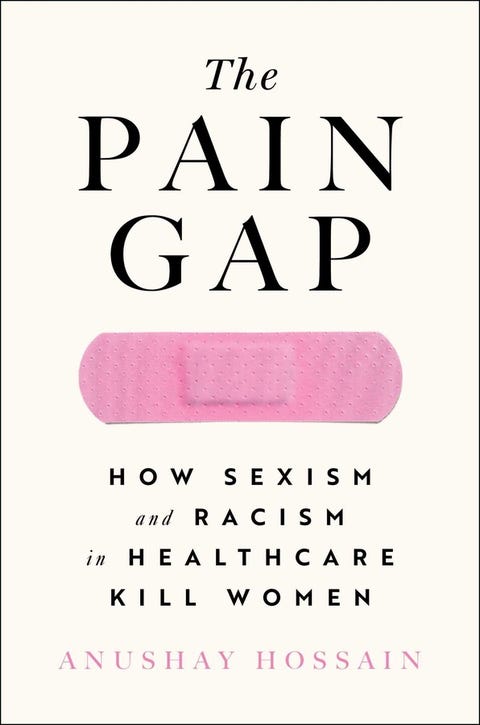
While the United States was already in the midst of a maternal health crisis before the pandemic hit, for women of color, especially Black women, things went from bad to worse. It’s an ongoing health scandal we should all be talking about more, and I hope that my new book, The Pain Gap: How Sexism and Racism in Healthcare Kill Women, will help start those crucial conversations.
Women of color are currently two to three times more likely to die giving birth in America, but it is Black women who are paying the highest price. Studies show that they are 243 percent more likely to die than their white counterparts: They have a death rate of 40.8 per 100,000 births, while white birthing people have a rate of 14.7 per 100,000. Black women are also more likely than Asian or Latina women to die from pregnancy-related complications regardless of their education level or their income.
We know that the majority of these women are dying needless, preventable deaths, because we have the medical expertise to prevent and manage pregnancy complications. So why is this crisis ongoing?
The reasons, of course, are complicated. Black Americans are infected with COVID-19 at nearly three times the rate of white Americans, and studies show that the virus is even deadlier during pregnancy. What’s more, during the early days of the pandemic, many hospitals implemented the “one-person policy,” a rule that allowed only one person to attend a birth, making pregnant women choose between family members, increasing their isolation. This policy disproportionately impacted women of color, especially Black women, who are more likely to hire a doula to advocate on their behalf and provide support during labor.
Of course, racial disparities in risk factors related to pregnancy such as hypertension, anemia, and gestational diabetes also play a big role, and are worsened by stress related to racial inequality and health care, which skyrocketed during the pandemic.
Even before COVID-19, Black mothers reported that their pain and concerns were routinely dismissed by medical professionals. Tennis superstar Serena Williams almost died after her C-section in 2017 when pain in her lungs indicated that she could’ve had a blood clot. Williams had to fight to convince hospital staff to check it out, and when they did, she was returned to surgery where the doctors indeed found a large hematoma, a swelling of clotted blood.
“For years, there has been implicit racial bias in American medicine,” Mary Rosser, director of Integrated Women’s Health at Columbia University Irving Medical Center in New York City, says. “America has segregated people into neighborhoods where they don’t have access to resources such as healthy food, green spaces, job opportunities, good housing, and health care. This is compounded with the stress caused by structural racism, which also impacts Black women’s health.”
A 2016 analysis of five years of data found that Black, college-educated mothers who gave birth in local hospitals were more likely to suffer severe complications during pregnancy or childbirth than white women who never graduated from high school. This proves that even education cannot protect Black women from the risk of dying while giving birth in America, because the health care system treats people differently based on race.
Joia Crear-Perry is a physician, policy expert, and founder and president of the National Birth Equity Collaborative (NBEC). She is also on the advisory board of Black Mamas Matter Alliance, a national network of more than two dozen maternal health initiatives and organizations led by Black women. Crear-Perry points out that factors leading to these alarming statistics for Black women are not based on DNA.
“We’re not biologically different; there’s no Black gene or Black heart or Black kidneys,” she said in a recent interview with American Heart Association News. “We’ve spent generations blaming Black people for their outcomes without really addressing the underlying root causes of racism, classism and gender oppression. So, when people ask me what is the cause for Black maternal death, the answer is not race. It’s racism.”
Maternal mortality numbers are also horrific for Native women in America, who make up the second most at-risk group after Black women. In 2017, Native women died during childbirth at a rate of 28.3 deaths per 100,000 live births, which was more than double the rate of white women. While women in the United States today are 50 percent more likely to die in childbirth than their mothers, that risk is three to four times higher for Black and Indigenous women.
As pointed out in a 2015 report published by The International Journal of Gynecology & Obstetrics, American Indian/Alaskan Natives suffer from “unique health disparities,” and while the reasons remain unclear—experts have demanded more research—this ethnic group sees higher rates of obstetrical complications such as preterm birth and postpartum hemorrhage.
A 2020 report from the Center for American Progress states that “the coronavirus pandemic has thrown the shortcomings of the U.S. health care system into stark reality,” and that the “compounding public health crises of the coronavirus and racial disparities in maternal mortality only exacerbate the strain on the health care system and the risks for those most vulnerable, particularly women of color.”
Ten years ago, I experienced this type of discrimination firsthand when I almost died in childbirth. I am still not over the shock. I was ready for childbirth to be the most empowering experience of my life, but instead, I was forced to confront the real possibility that the color of my skin played a role in the way I was treated at the hospital. The experience put me on a journey to understand how a privileged, highly educated Bangladeshi woman like me almost died giving birth in America.
While we deal with our cultural hard truths, the good news is that we can take political action right now on Capitol Hill. President Joe Biden’s Build Back Better legislation includes comprehensive investments from the Black Maternal Health Momnibus Act, including funding to address social determinants of maternal health, investments to grow and diversify the perinatal workforce, and resources specifically for community-based organizations and maternal mental health equity grant programs. The Build Back Better Act also includes an evidence-based mandatory provision that will make federal funds permanently available for states to expand postpartum Medicaid coverage to one year.
We must call and urge our representatives in Congress to ensure that these key maternal health policies are signed into law. It is crucial to raise our voices to demand policy change that centers Black birthing people, for they are the face of America’s maternal health crisis. And that’s a reality we all have the power to change.