The devastation wrought by the worst recorded Ebola outbreak in history grows daily. As of Thursday, the deaths totalled 729 deaths in West Africa, according to the World Health Organization (WHO), but it's far from over; "Ebola is worsening in West Africa," CDC director Tom Frieden said not once, or twice, but three times on Thursday.
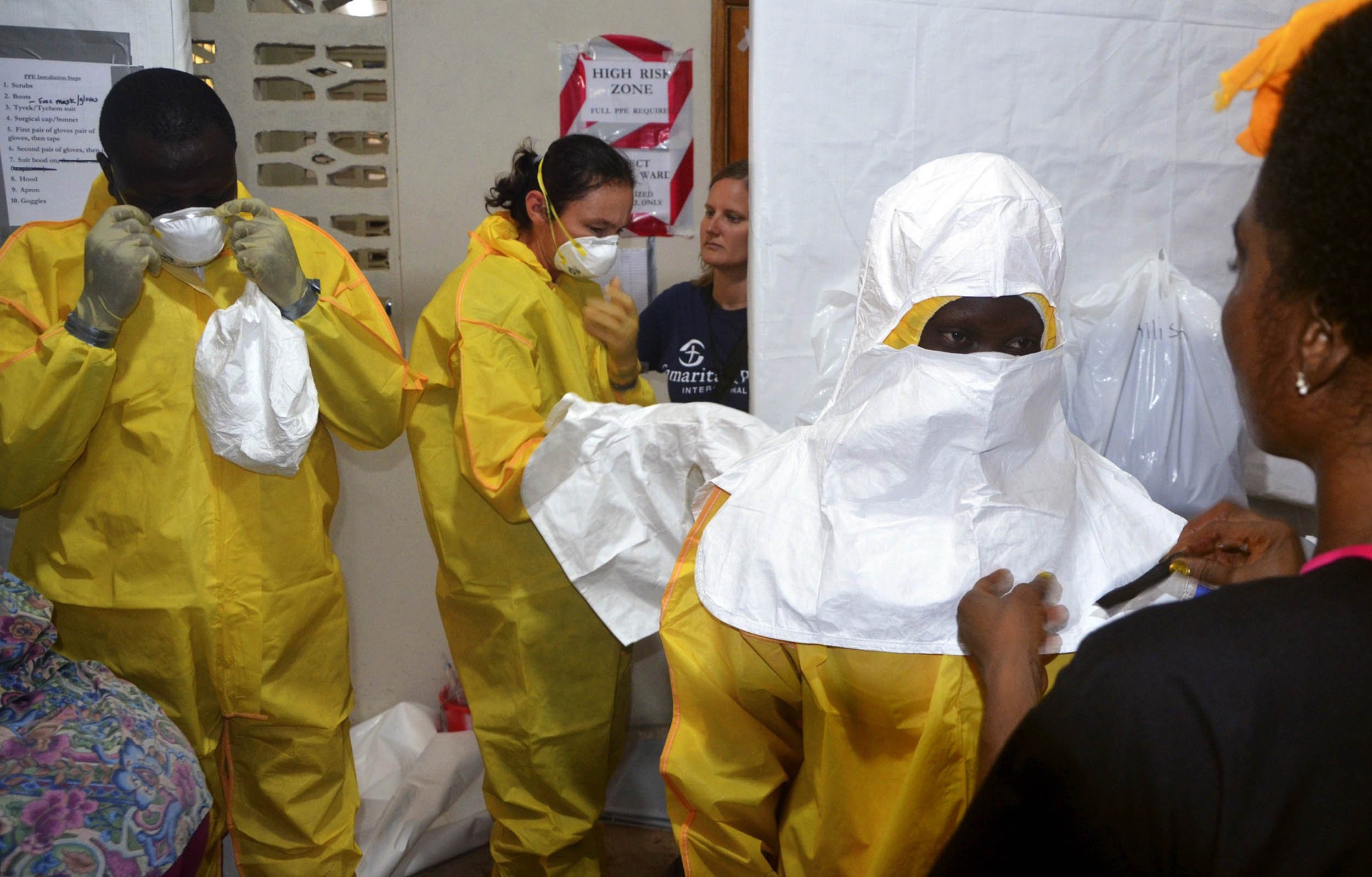
Infectious disease experts are mobilizing, borders are shutting down, and, despite the fact that there is no cure for Ebola haemorrhagic fever (the illness caused by Ebola virus infection), health care officials are trying anything they can to help the stricken—especially those who put themselves at risk to save others. That means digging deep into the list of experimental methods the WHO, CDC and others have developed over the past few years to cure the deadly viral infection—including a simple but controversial therapy called immune plasma infusion.
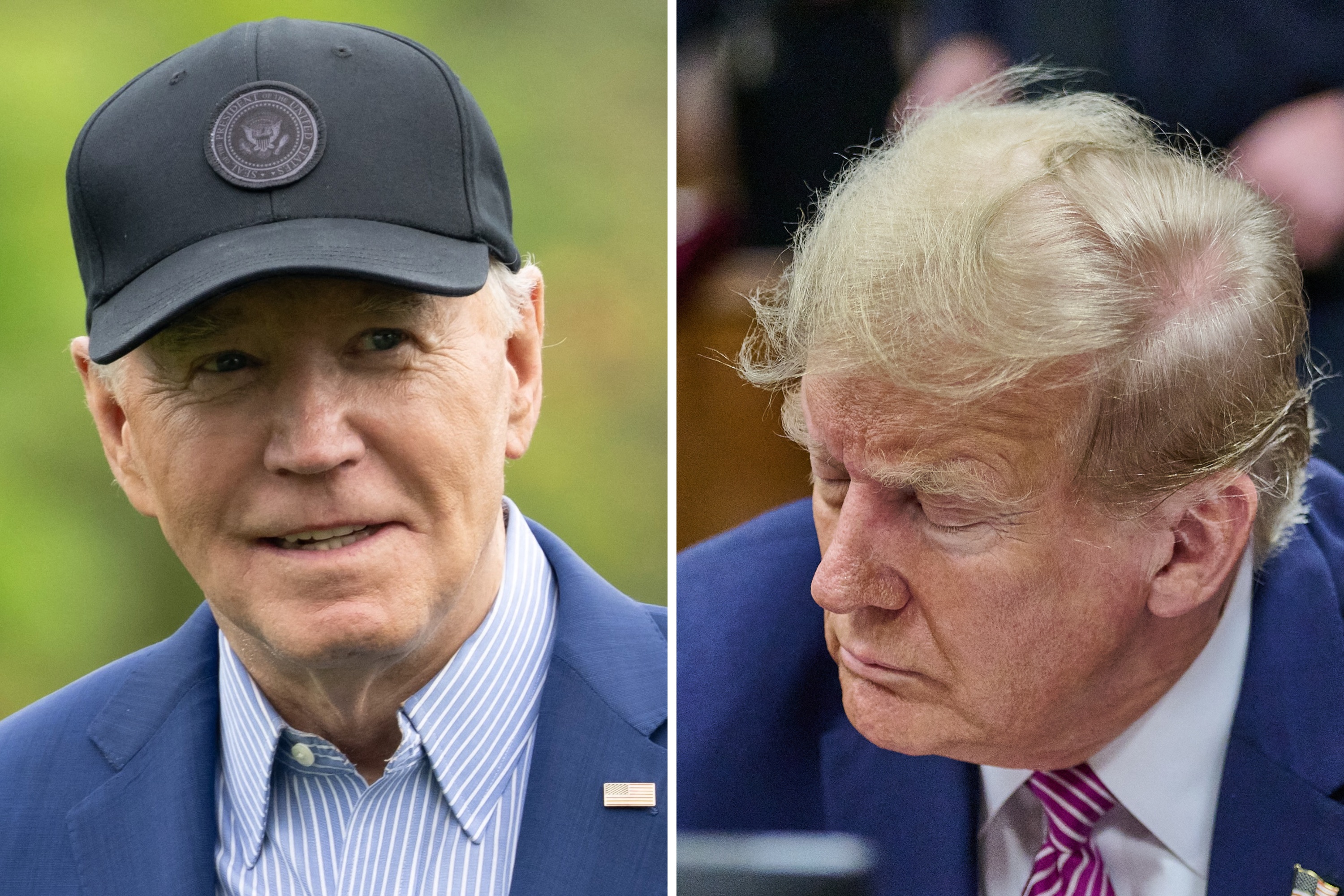
In Monrovia, Liberia, 33-year old Dr. Kent Brantly of Forth Worth, Texas had been treating Ebola patients since June, as part of an international relief group called Samaritan's Purse. But in mid-July, Brantly recognized that he himself was showing symptoms of Ebola. He isolated himself, and told the rest of the team of his suspicions; soon after, his diagnosis was confirmed.
On Thursday Brantly was given a shot at survival: a 14-year-old male Ebola patient who had been under Brantly's care, and survived, donated a "unit of blood" to Brantly, according to Samaritan's Purse President Franklin Graham. "The young boy and his family wanted to be able to help the doctor that saved his life."
The idea—novel, though not unprecedented—is that the blood (plasma, in medical parlance) of a survivor, full of antibodies proven to be strong enough to fight off the disease (i.e., immune), when transfused into an infected body, might help that body become immune itself. Though it sounds a bit like something Hollywood might have cooked up, there's some science behind it—and an historical precedent that offers hope.
***
By the time Robert Colebunders arrived in Kikwit, Democratic Republic of Congo (known as Zaire at the time), on June 15 of 1995, the Ebola virus had ravaged the city of 250,000 and the neighboring area for nearly 6 months. The hospitals in the riverport town were empty; patients and healthcare workers had fled to other parts of the country for fear of contracting the deadly disease, which would ultimately affect 317 people and kill 245.
Eventually, the Kikwit Ebola outbreak was traced back to January 1995, but it wasn't until the start of May of that year that local public health officials recognized the many sick patients in the area as victims of the infectious disease. On May 8th, the Zairian government officially declared the epidemic, asking the World Health Organization to mobilize international assistance. Soon after, infectious disease experts arrived from the WHO, the CDC, Doctors Without Borders, the South African Medical Institute, the Red Cross, and Belgium's Institute of Tropical Medicine—which sent Colebunders.
Immediately, the team went to work to contain the disease.
"We rapidly began talking to local leaders, quickly helping create an understanding in the population that an intervention was needed," says Colebunders. The team established a surveillance network to identify and isolate patients who were suspected to have Ebola, and distributed protective equipment that gave local health care workers the ability—and the confidence—to safely work with the infected.
"We buried the dead bodies ourselves," says Colebunders, working with Red Cross volunteers. Not just the known Ebola victims, either; every dead body in the area. The traditional burial rituals in the area involve family members cleaning the dead body, mourners coming to touch and kiss the body, and even keeping hair and nail as souvenirs. "If its not done in the right way, they think the ghost of the person will do them some harm," says Colebunders. They had to convince them to put the bodies in plastic bags, a hard sell anywhere. "Putting your loved one in a plastic body bag is really not acceptable. That's for your trash," Colebunders says. "You need to help them understand."
It worked: soon enough, reports of newly infected patients petered out. They were near declaring victory.
Then, in the last days, a nurse at Kikwit General Hospital, who had volunteered to care for a pair of Ebola-infected Italian nuns, developed symptoms of Ebola hemorrhagic fever.
"The rest of the team became concerned," says Colebunders, and some of the medical professionals there who had suffered through and survived an earlier infection ("convalescent patients" in the literature) wanted to donate some of their blood to the nurse. "The Americans and Scientists from the States didnt believe it could work," says Colebunders, but the Congolese doctors did it anyway. The same blood transfusion procedure was repeated for seven others who were ill, the final group of Ebola-stricken patients in the hospital.
The results were staggering: seven of the eight survived.
Typically, Ebola is almost unbelievably deadly; some strains kill almost 90 percent of those they infect. It's "very dramatic and even preternatural," says David Quammen, a journalist and author of Spillover, a book documenting the impact of zoonotic diseases like Ebola. "It kills people quickly and it kills a high proportion of the people it infects." The Kikwit case study (which would go on to be published in the Journal of Infectious Diseases) showed an almost 90 percent survival rate.
There's precedent for this treatment approach, too. "We use this in other infectious diseases, and we can—and should—use that experience and apply it to Ebola," says Heinrich Feldmann, the head of the National Institute of Health's Laboratory of Virology. In Argentina, for example, infection of the Junin virus is often (and effectively) treated with blood transfusions from a Junin survivor.
So, why hasn't the CDC, the WHO and the rest of the public health organizations worldwide jumped all over immune plasma infusion for Ebola? Why are we still scrambling for an Ebola treatment 20 years later?
The answer is that it has been essentially impossible to test. Why? Because Ebola only pops up occasionally, infects a relative few, and kills most. There's no way, says Feldmann, to get enough plasma during an outbreak to treat others involved in that same outbreak. "Of course if you are collecting plasma now for the next outbreak, then you will have the time to do it," Feldmann adds, though he is unaware of anyone collecting plasma during the current West African outbreak.
At least, until the unnamed 14-year-old boy, who, of his own accord, is about to become a key piece of the second test case in 20 years for what could be the treatment we've all been waiting for.
"We clearly need more effective ways to treat these patients and to protect health care workers," says Colebunders. "Confronted with such a deadly disease, it is time to consider the use of experimental vaccines and treatments as compassionate use."
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
Elijah Wolfson is a Senior Editor at Newsweek, where he writes and edits on science, health, technology and culture. He is ... Read more
To read how Newsweek uses AI as a newsroom tool, Click here.