Surgery. Radiotherapy. Chemotherapy.
Those are the cancer treatments most of us are familiar with, and in many cases, even all three combined are not enough to provide a complete cure. But a new and innovative approach may enable oncologists to add another option to the list. An artificial magnetic bacterium was recently created in a Spanish laboratory that, when ingested, can work as a magnetically charged compass that targets tumors and destroys them by spinning so fast the tumors heat up and melt.
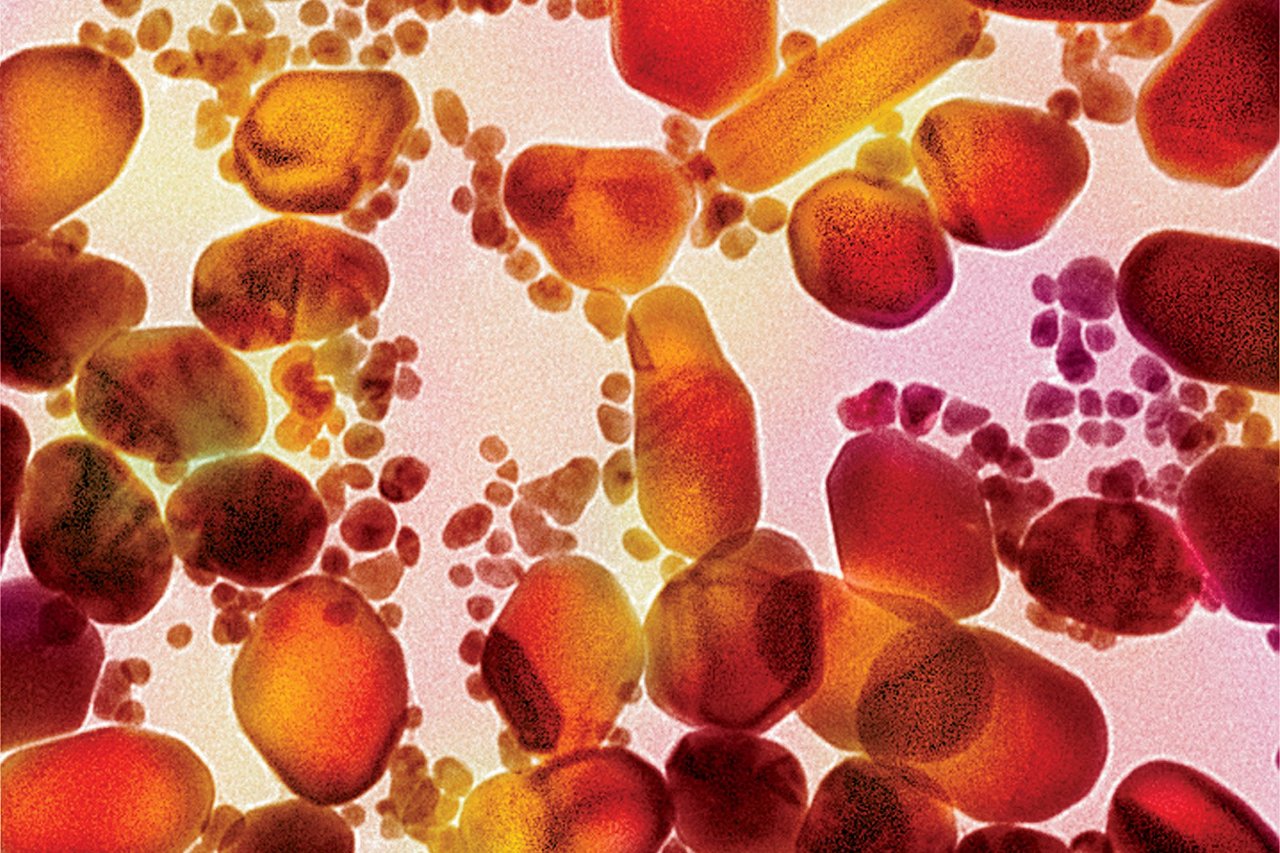
It's based on an experimental treatment methodology called "magnetic hyperthermia" that exposes tumors filled with magnetic nanoparticles to an alternating magnetic field. So far, most tests have been on cancer-stricken mice.
The first step is to flood a tumor with magnetic materials, like iron nanoparticles. All of the body's cells need oxygen to function—without oxygen, a tumor couldn't grow larger than a grain of sugar, so it sends out hormone signals that allow it to hijack nearby blood vessels, which can then deliver oxygen-rich blood directly to it. However, because the blood vessels inside tumors grow in a rapid and disorganized way, they tend to be faulty and leaky.
If you inject magnetic iron nanoparticles into the bloodstream, they circulate throughout the body, bypassing the healthy blood vessels until they find entryways through the leaky ones that feed the tumor. Ultimately, iron nanoparticles will travel until they find a tumor's blood source, feed the tumor iron-laden blood and accumulate there. (It takes 24 hours for iron to fill up mice tumors; it would likely take longer to move through the human body, which has a much larger circulatory system.)
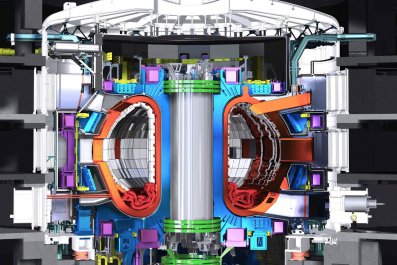
Then the patient lies in a magnetic resonance imaging (MRI) machine, where tumors can be heated up to 150 degrees Fahrenheit in just two minutes. The iron nanoparticles inside the tumor spin rapidly from the opposing magnetic poles of the MRI scan—think of what happens when you try to hold two repelling magnets next to each other. This generates heat, and once the tumor reaches temperatures of 104 degrees Fahrenheit for 60 to 90 minutes, its cells begin to break down and liquefy.
Though experiments on both lab mice and even humans in Europe have shown some successes, the challenge now is in the delivery system: Iron nanoparticle injections move throughout the body's bloodstream and become diluted, making it difficult to build up the iron levels needed to destroy the tumors.
So researchers from the University in Granada, Spain, designed digestible magnetic bacteria that could leak through the lining of the stomach in order to quickly fill local stomach tumors with iron. Patients would only have to eat yogurt or other foods laced with probiotic bacteria, and wait three hours for it to digest, to get the first step of the treatment out of the way.
Jose M. Dominguez-Vera, the lead researcher on the project, says his team has already tested the artificial bacteria in animals. The next step will be to find the right concentration of magnetic bacteria that will enable it to target tumors of the human digestive tract without harming the patient.
That's the same challenge James Hainfeld, an adjunct professor of biomedical engineering at Stony Brook University and president and chief scientist of Nanoprobes Inc., encountered. After 30 years of exploring magnetic hyperthermia, Hainfeld learned that scaling up from mice to humans is particularly difficult because of "background heating." In the human body, each molecule has its own specific absorption rate due to different degrees of magnetism, which heat up atoms to varying temperatures. Water molecules, for example, heat up, while calcium doesn't at all. Mice have different levels and concentrations of molecules than humans do, making it harder to predict how humans will handle cancer-treatment trials that have been tested on the much smaller rodents.
The trick is getting the iron particles hot enough to destroy the tumor without raising the temperatures of—and, therefore, damaging—healthy cells. Researchers also have to be careful not to add too much iron, because at high levels the metal can become toxic to the body and cause heart and liver tissue damage. The accumulation of too much iron in organs can lead to chronic fatigue, weakness, joint pain, abdominal pain or organ damage. And if iron overload goes untreated, it can cause infertility, heart disease, liver cancer or diabetes, among other medical conditions.
But if scientists can overcome these problems, those iron particles might turn into a silver bullet for cancer. Hainfeld found that when tumors were treated with magnetic hyperthermia, they became three to four times more vulnerable to cancer treatments such as radiation therapy. This could be a game changer, as there is a lifetime cap on the amount of radiation the human body can handle; by pretreating tumors, lower dosages of radiation would be needed to destroy tumors. Lung cancer patients, in particular, could benefit tremendously from the treatment.
"[Lung cancer] is mainly untreatable now only because radiation can't be used over such a large area. This could fix that," says Hainfeld.
In addition, the method can be used in a much more targeted way than traditional cancer treatments. "Magnetic hyperthermia is engineered to be effective with solid tumors of any kind, anywhere in the body," says Hainfeld. "We can then turn on an otherwise harmless alternating magnetic field, and all those tumors will just cook to death—while adjacent tissue is cleanly spared."
Brain tumors are another scourge that magnetic hyperthermia might address. They are often irregularly shaped, making it a challenge to surgically remove all cancerous cells. As a result, 76 percent of people with primary brain tumors die within five years of diagnosis. It can be virtually impossible to surgically remove an entire brain tumor, Hainfeld says, but sending magnetic nanoparticles into tumors through the bloodstream and then heating them up with radiation could work.
Before Hainfeld started experimenting with iron, he attempted to flood tumors with a different nanoparticle: gold. He found that mice with brain tumors that were given IVs of gold nanoparticles had a 56 percent survival rate when treated with radiation therapy—compared with only 18 percent in the control group.
But Hainfeld says that funding for this type of work has been scarce, and trials in the U.S. have yet to move past in vivo animal testing. The U.S. Food and Drug Administration (FDA) says that if a gold or iron nanoparticle treatment was shown to be effective in human trials, it would consider granting approval.
"If the review of the data show the drug's potential benefits outweigh its risks, it receives approval and can be marketed for use in the United States," says FDA press officer Stephanie Yao.
Hainfeld believes that's likely to be the case. "If somebody's going to die of cancer, if you've got a few particles in your liver, then so what," he says. "Cancer is a vicious, horrible disease, and if something helps, it may be worth doing."